Summary: If you want to understand the promise of AI/ML in healthcare you need to see it through the eyes of physicians, the ultimate users. Turns out these folks aren’t the rapid adopters you’d think they’d be and the problem is largely with the way data scientists have tried to implement. Part 1 of 3.
 It’s hard to write about AI/ML in healthcare, at least fairly. You wouldn’t think so given the number of over-the-top articles on the spectacular promises that AI/ML hold in this field.
It’s hard to write about AI/ML in healthcare, at least fairly. You wouldn’t think so given the number of over-the-top articles on the spectacular promises that AI/ML hold in this field.
The core of the problem is that these articles are all written from a data science point of view about what’s possible but not from the perspective of the doctors and clinicians who must adopt these breakthroughs.
This last December I attended a three-day AIMed conference and as the name implies this is all about the impact of AI/ML in healthcare. The difference is that instead of being attended by data scientists, 80% of attendees were either clinicians or hospital CIO/Administrators. These folks are definitely not data scientists. They are the users and beneficiaries of AI/ML tools and techniques.
They are also the earliest of adopters, or at least those open to the idea. And while there was a great deal of enthusiasm, indeed almost cheerleading, the message in almost every presentation was that AI/ML may be coming but it’s not ready for prime time in healthcare.
Only 1% of US Hospitals Have Data Science Programs
In fact, a statistic offered by the founder and leader of this conference, Dr. Anthony Chang, with the unique credentials of being a practicing cardiologist, a trained data scientist, and Chief Intelligence/ Innovation Officer for his hospital is that only about 1% of the roughly 5,500 US hospitals have active data science programs. The fact that only about 50 hospitals in the US have such a program was validated by a number of other attendees.
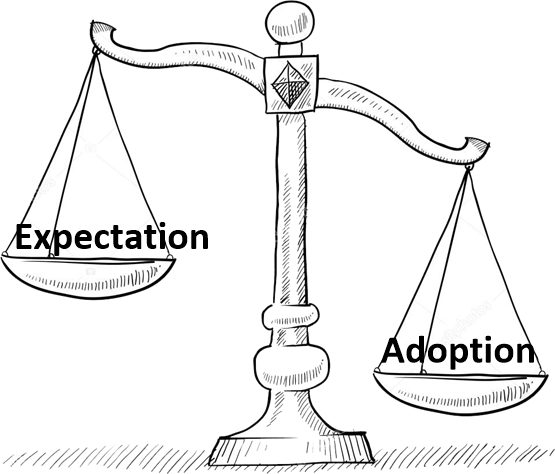 Nowhere else in the public or private sector is there such an imbalance between adoption and expectation.
Nowhere else in the public or private sector is there such an imbalance between adoption and expectation.
This 1% penetration compares to between 20% and 33% of larger corporations who are sponsoring full-on programs to remake themselves with AI/ML tools, and the better than half, perhaps as many as two-thirds of large and mid-size companies that have at least some reasonable project underway.
Frankly you have to come away from such an experience with the feeling that 99% of clinicians welcome AI/ML driven change as much as a fish needs a bicycle.
Causes of Slow Adoption
What I learned from these mostly user presentations is that the root causes of this slow adoption is partially financial, but most important for the readers of this article, because of the hubris of we practicing data scientists. This includes particularly the hundreds of AI/ML healthcare startups and big-tech innovation labs looking to follow the path of disruption to financial success and glory.
Let me be clear. It remains true that perhaps the greatest good that AI/ML will achieve over the next 10 or 20 years lies in improving the health and wellness of every human being.
But to get there we who are creating these tools and techniques have many lessons to learn about the unique nature of healthcare, both in the US and abroad.
More specifically we need to understand the unique workflows and processes of clinicians and how our AI/ML tools need to integrate.
The Big Picture
There are almost as many ways to parse these AI/ML opportunities as there are authors who write about them. In part 2 we’ll take a slightly different perspective to this slice and dice focusing first based on who pays, and then on the patient’s experience of the medical process.
The top line groups from the patient’s and doctor’s perspective are:
- Drug discovery and innovation
Of all the AI/ML opportunities in healthcare this one is actually furthest along largely because it’s big pharma that pays, not the insurers.
- The business of healthcare
The operational world of the clinician may be unique but at a business level hospitals and healthcare organizations share some marked similarities with the commercial world.
- Patient intake and referral
Determining whether and when a patient gets to see a doctor is a major control point for constraining healthcare costs, especially in single payer systems. The initial consult with the doctor is also a major time sink that could be at least partially automated.
- Clinical applications – what happens between clinician and patient. AKA the AI/ML augmented physician.
If you want AI/ML to succeed in improving healthcare it needs to get into the space between the doctor and the patient. Several major subsets of this opportunity need to be understood separately.
4.1 Automated / Semi-automated interpretation of medical images.
4.2 Enabling more accurate identification of disease subtypes – precision medicine.
4.3 AI/ML driven triage and prevention including:
4.3.1 Models to identify and develop protocols that result in better outcomes.
4.3.2 Models focusing on triage and prevention of bad outcomes.
4.3.3 Models focusing on anomalies and types of preventable harm.
- The Profit Motive and Sharing Savings
No conversation of AI/ML adoption would be complete without understanding how the complex financial reimbursement world is changing to a shared savings model.
- Creating accurate data – the Electronic Health Record (EHR)
Finally, how data is created, shared, utilized, and perhaps most importantly why the EHR is driving physicians to distraction.
Financial Considerations
Before we get into the meat of this topic let’s acknowledge that hospitals and healthcare practices come in all sizes. Certainly not all of the roughly 5,500 hospitals in the US (2018) are large enough to have data scientists on staff. Some teeter on the edge of unprofitability and may not be able to adopt even packaged AI/ML systems despite the benefits. About 20% are federal or state owned which comes with its own set of purchasing and innovation challenges.
Still with commercial adoption of AI/ML in the range of 20% to 33% of medium and large companies, we might have expected more like 500 to 1,500 hospital adopters instead of the roughly 50 to 60 that exist.
So finance, while a real consideration, doesn’t explain the low and slow adoption rate.
The promise of AI/ML in healthcare remains very high but adoption remains low and slow. The landscape is more complex than you might imagine. And there are very important lessons here for those data scientists hoping to bring AI/ML to healthcare without appreciating the huge difference in cultures. Those lessons are of value to all of us, regardless of which industries we focus on.
In the balance of this three-part series we’ll offer more detail on the opportunities in each segment and where AI/ML is succeeding and can succeed in the short term.
Perhaps the more important new news will come in the third part and speaks specifically to the many barriers that are holding back adoption.
Other Articles in this Series
The AI/ML Opportunity Landscape in Healthcare. Do It Right or It Will be More of a Mine Field
Doctors are from Venus, Data Scientists from Mars – or Why AI/ML is Moving so Slowly in Healthcare
Other articles by Bill Vorhies.
About the author: Bill is Editorial Director for Data Science Central. Bill is also President & Chief Data Scientist at Data-Magnum and has practiced as a data scientist since 2001. He can be reached at:
