AI technology is reshaping healthcare by streamlining the process of providing patient care. For example, it can deliver test results faster and more accurately than before.
It also helps with clerical tasks, insurance appeals, and claims processing. This automation can reduce human error, ensuring patients receive the necessary care.
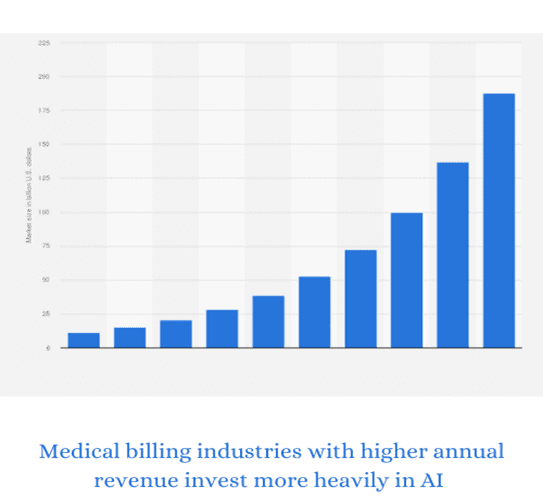
By increasing productivity, lowering errors, and lowering costs, Artificial Intelligence (AI) is transforming medical billing. Several ways in which Artificial Intelligence (AI) is transforming medical billing include:
1. Accurate Claims
AI technologies like machine learning (ML) and natural language processing (NLP) are used in medical billing to improve the accuracy of claims. These systems can also help reduce the risk of human error by correcting errors found in transcriptions and validation checks.
One way to ensure accurate coding is to digitise original claims from hospitals and medical practitioners. This means capturing and storing data in digital form for the AI system to use.
Another way to ensure accurate coding is to automate processes. ML tools can be used to analyse and extract medical data from insurer web portals, Electronic Medical Record (EMR) systems, billing software, scanned documents, etc. These AI solutions can help medical professionals reduce the time and effort needed to code patient encounters.
2. Better Patient Care
AI is reshaping the healthcare industry by improving patient care, reducing costs, and providing accurate health data reports. Specifically, AI is helping to increase patient engagement and adherence.
For example, AI-powered applications can help care teams identify potential non-adherence issues early on, allowing them to intervene before it becomes a patient problem.
Furthermore, AI can also help doctors streamline certain aspects of patient visits. This will reduce administrative tasks, allowing doctors to spend more time with their patients and provide them with better medical care.
While AI can potentially change the healthcare industry, it will require careful consideration and thoughtful policy for many years. Some of the key challenges include algorithmic limitations, misalignment of incentives, and regulatory barriers. These challenges must be addressed to ensure the best possible results for all stakeholders.
3. More Time for Doctors
Medical billing and coding are complex processes that require a lot of attention to detail. These tasks can be costly for hospitals and clinics if errors are made during the process.
However, these issues can be resolved quickly and accurately with the right AI-powered solutions. These technologies also can identify fraud, waste, and abuse.
This is essential for health systems, plans, and PBMs to focus on. As a result, they can improve their bottom lines while improving the quality of care and patient experience. These new solutions can also help them stay competitive in a rapidly evolving healthcare landscape.
4. Better Reimbursement
One of the ways that AI is reshaping medical billing and insurance is by providing better reimbursement for hospitals and clinics. This is because AI can help to analyse data and identify any errors that may be present in insurance claims. This can then be used to correct the errors before they are sent to the insurance company, saving both the hospital or clinic and the insurance company time and money.
AI is also helping to improve patients’ financial experience by allowing them to see how much their visit will cost before they go. This is something that many patients want, making seeing a doctor much more manageable.
5. Reduced Costs
Across the health industry, AI solutions are being implemented to make workflows more efficient. This is particularly true in the medical billing arena, which can be an expensive and repetitive process for both providers and insurers.
One major challenge is the accuracy of coding. Incorrect codes can lead to rejected claims and a loss of money for both parties.
But AI can improve coding accuracy by analysing doctors’ notes and insurance policies. It also can extract data from insurer web portals, EHRs, and other systems.
This makes it easier to provide accurate patient eligibility estimates. It also saves practice time, as they no longer need to check multiple systems for each patient. This helps reduce patient cancellations and improves point-of-service collections. It also helps with patient financing and provides patients with a better understanding of their out-of-pocket costs before receiving care.
